Spring is in the May air and my next blog has come round quickly after a busy month!
Following on from last month’s blog on heart failure disease register validation and essential to-do’s on clinical coding; I thought heart failure medication optimisation would be appropriate.
Patients with Heart Failure with Reduced Ejection Fraction (HFrEF), or more commonly known as Left Ventricular Systolic Dysfunction (LVSD), should be treated systematically adhering to the 4 pillars of heart failure management.
So, what are the 4 pillars of heart failure management?
Basically, the 4 pillars is a quadruple medication approach, as described in the European Society of Cardiology (ESC) (McDonagh et al. 2021) guidelines, for managing HFrEF, as listed in the figure below:
Strategic Phenotypic Overview of the Management of HFrEF
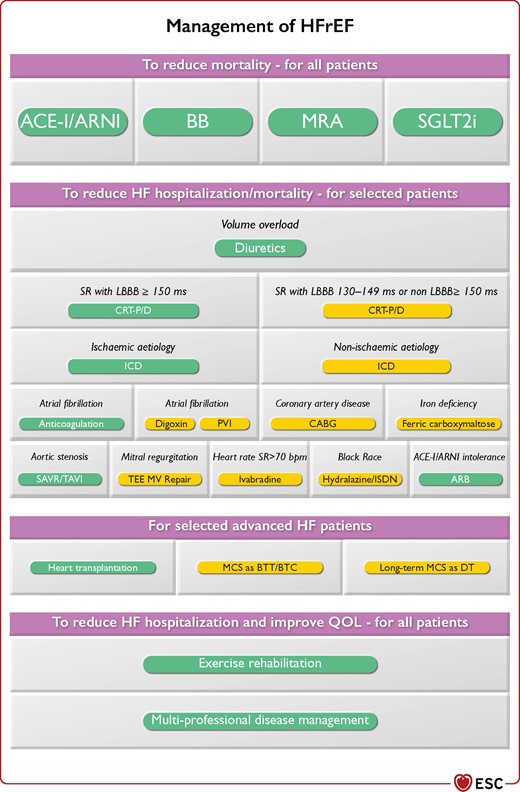
Strategic phenotypic overview of the management of heart failure with reduced ejection fraction. ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker; ARNI = angiotensin receptor-neprilysin inhibitor; BB = beta-blocker; b.p.m. = beats per minute; BTC = bridge to candidacy; BTT = bridge to transplantation; CABG = coronary artery bypass graft; CRT-D = cardiac resynchronization therapy with defibrillator; CRT-P = cardiac resynchronization therapy pacemaker; DT = destination therapy; HF = heart failure; HFrEF = heart failure with reduced ejection fraction; ICD = implantable cardioverter-defibrillator; ISDN = isosorbide dinitrate; LBBB = left bundle branch block; MCS = mechanical circulatory support; MRA = mineralocorticoid receptor antagonist; MV = mitral valve; PVI = pulmonary vein isolation; QOL = quality of life; SAVR = surgical aortic valve replacement; SGLT2i = sodium-glucose co-transporter 2 inhibitor; SR = sinus rhythm; TAVI = transcatheter aortic valve replacement; TEE = transcatheter edge to edge. Colour code for classes of recommendation: Green for Class of recommendation I; Yellow for Class of recommendation IIa (see Table 1 for further details on classes of recommendation). The Figure shows management options with Class I and IIa recommendations. See the specific Tables for those with Class IIb recommendations at https://academic.oup.com/eurheartj/article/42/36/3599/6358045
Primary care has become somewhat more familiar with ACEi (e.g. Enalapril) and beta-blocker (i.e. Carvedilol, Bisoprolol, Nebivolol) therapies over the years, with the MRA (Spironolactone/Epleronone) medication group becoming more widely recognised as triple therapy for patients with HFrEF.
However, much has changed and we now have more superior treatment in replacement of an ACEi/ARB for specific patients such as the use of ARNI, i.e. Sacubitril Valsartan (NICE, 2018; McDonagh et al. 2021).
In addition to triple therapy, we have seen a fourth medication added to the medication regime.
SGLT2i (such as Dapagliflozin and Empaglifozin) are now recommended as a quadruple therapy in HFrEF.
This medication adds further morbidity and mortality benefits. (McDonagh et al. 2021); Straw et al. (2021).
Vaduganathan, et al (2020) report that the average 65-year heart failure patient could expect up to an additional 5 years if receiving the 4 pillars of treatment.
With my primary care hat on, I am seeing more and more patients receiving quadruple therapies, which is reassuring, but we have a long way to go to ensure this is accessed equitable and systematically among general practice patients.
Secondly, medication optimisation, i.e. titration to optimally tolerated dose or target dose, should be being focussed upon in a heart failure review consultation in general practice.
It goes without saying, some patients can be complex and require more close assessment and guidance in terms of priority ordering of the 4 pillars of treatment and referral to our cardiology heart failure team is advised.
Nonetheless, much can be achieved in primary care clinic at the patients 6/12 monthly review.
For practices using the Quality & Outcomes Framework (QOF) it is expected that a heart failure medication review is an ideal time to identify patients who require medication optimisation.
I can hear you say; “But what will patients say when all of a sudden, we begin to titrate their medication now and not before.”
Be candid; general practice is diverse and we have an expanding knowledge base on what we can do for patients with HFrEF, and most patients won’t question that fact.
Don’t let status quo stop you optimising their medications.
I can hear you say, “I’m not a heart failure expert”, well I appreciate that, but many patient’s medications can be easily titrated and it’s not as hard as you think!
Many primary care colleagues are now using mentoring with a local heart failure nurse, advanced pharmacy practitioner, GP with special interest cardiology/HF to increase confidence and competency.
Nationally, there has been access to a fully funded foundation in HF webinar course. There are many available courses to help brush up your heart failure knowledge and skills.
Don’t forget, heart failure audit is key place to begin with primary care heart failure management.
For example, the Oberoi Disease Management Audit Platform (oberoi-dm.co.uk) supports primary care to identify diagnostics coding issues, identify missing heart failure patients and clearly identifies patients who are not taking therapies for HFrEF and those who require medication optimisation.
If you would like to discuss heart failure audit, coding and or your educational requirements please feel free to email me on: Amanda.Crundall@oberoi-consulting.com
McDonagh et al. (2021). ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal. Sep 21; 42 (36): 3599-3726. https://pubmed.ncbi.nlm.nih.gov/34447992
NICE (2018) www.nice.org.uk/guidance/ng106
Vaduganathan et al. (2020) Estimating lifetime benefits of comprehensive disease-modifying pharmacological therapies in patients with heart failure with reduced ejection fraction: a comparative analysis of three randomised controlled trials. Lancet 2020; 396:121–8.
Straw et al (2021) Four pillars of heart failure: contemporary pharmacological therapy for heart failure with reduced ejection fraction. British Medical Journal. http://dx.doi.org/10.1136/openhrt-2021-001585

